In the soft flicker of tea lights against the walls of a cozy family home, Jennifer “Jen” Cahill, a 34-year-old mother of boundless resolve, labored through the night of June 2, 2024. Surrounded by lavender oil’s calming scent and a curated birthing playlist, she chased a vision of the perfect home birth for her second child, a daughter named Agnes Lily – a name evoking wildflowers and timeless grace. Jen’s birth plan, a 40-page manifesto crafted over months, was a testament to her fierce autonomy: no interventions, no pain relief, a water birth in an inflatable pool she’d set up herself, immediate skin-to-skin contact, and a sacred space free from hospital sterility. Her midwife, Sarah Fielding, called it “the most intense birth file I have ever read.” But what began as an empowering reclamation of motherhood ended in unthinkable tragedy. Within days, Jen and tiny Agnes would succumb to complications, leaving behind a grieving husband, Rob, and their three-year-old son, Rudy, adrift in a world forever dimmed. As an inquest unravels this devastating loss, questions burn: Did Jen’s meticulous plan reflect maternal strength, or did it mask risks overlooked in a strained healthcare system? This is not just a story of grief – it’s a searing call to examine the fragile balance of choice and safety in childbirth.
Jen’s world was one of resilience and quiet rebellion. An international export manager for a Manchester firm, she thrived on order, her desk adorned with color-coded planners. At 31, she and Rob, a 36-year-old IT consultant known for his gentle humor, welcomed Rudy at North Manchester General Hospital. That 2021 birth was traumatic: a postpartum hemorrhage costing Jen over 800ml of blood, a painful episiotomy, and a tear worsened by Rudy’s 9-pound-2-ounce frame. The hospital’s revolving door of midwives left her feeling like a number, not a mother. “No single midwife stayed with her,” Rob testified at the inquest, his voice raw. “It was chaotic – different faces, conflicting instructions. Jen felt abandoned.” The experience seared into her psyche, fueling a vow: her next birth would be on her terms, at home, where she could control every detail.
When Jen learned she was pregnant with Agnes in late 2023, she threw herself into planning with characteristic precision. She devoured books like Ina May’s Guide to Childbirth and joined online forums like the UK Home Birth Support Group on Facebook, amassing 12,000 members sharing stories of empowerment. Her plan, shared with Fielding, a seasoned independent midwife, was exhaustive: dim lighting, a doula named Claire for emotional support, a TENS machine for pain, and a birthing pool warmed to 37°C. She outlined positions – squatting, kneeling – to avoid tearing, and insisted on delayed cord clamping. Rob, initially hesitant about home birth given her history, was swayed by Jen’s fervor. “She was so sure,” he said, clutching a photo of Jen laughing with Rudy at a park. “She wanted Agnes to enter the world in love, not chaos.”
Home births, while growing in popularity, remain rare in the UK, accounting for just 2.3% of deliveries in 2023, per NHS data. Jen’s high-risk status – her previous hemorrhage and tear – raised red flags, but she was undeterred. Fielding, with 15 years’ experience, assessed Jen’s health: blood pressure normal, no anemia, a healthy 37-week fetus. Jen declined hospital-based monitoring, citing distrust, though she allowed Fielding’s regular checks. “She was adamant about avoiding hospitals,” Fielding testified. “Her plan was meticulous, but it left little room for flexibility.” The inquest revealed Jen had researched every complication, scripting responses: if bleeding occurred, apply fundal massage; if labor stalled, try herbal tinctures. Yet her plan assumed a best-case scenario, a dangerous gamble for a high-risk pregnancy.
On June 2, labor began at 3 a.m. Jen, calm at first, swayed to Enya’s soothing melodies, the birthing pool shimmering under candlelight. Rob massaged her back, Rudy slept upstairs, and Claire whispered affirmations. By noon, contractions intensified, but Jen refused to deviate from her plan, declining Fielding’s suggestion to transfer to hospital when progress slowed. “She was in her zone,” Claire recalled. “She kept saying, ‘I’ve got this.’” At 6:47 p.m., after 15 hours, Agnes was born in the pool, a 7-pound-6-ounce girl with a faint cry. Jen, beaming, held her daughter skin-to-skin, the room awash in relief. But within minutes, warning signs emerged: Jen’s breathing grew shallow, her pulse raced, and blood pooled beneath her. Fielding, alarmed, called 999, but Jen, weakening, refused to leave, clinging to her vision of recovery at home.
Paramedics arrived at 7:12 p.m., finding Jen semi-conscious, her hemoglobin plummeting from another hemorrhage – later estimated at 1,200ml. Agnes, too, was struggling, her oxygen levels dipping due to umbilical cord complications undetected in the home setting. Both were rushed to Royal Oldham Hospital, but Jen’s heart stopped en route; she was pronounced dead at 8:03 p.m. Agnes, placed in neonatal intensive care, fought for three days but succumbed to hypoxic brain injury on June 5. The coroner’s report listed Jen’s cause of death as postpartum hemorrhage compounded by uterine atony; Agnes’s as perinatal asphyxia. The inquest, opened in July 2024 and ongoing, probes whether timely hospital transfer could have saved them.
Rob, now raising Rudy alone, is haunted by what-ifs. “Jen was so strong, so sure,” he said, his voice breaking as he showed a photo of her cradling Rudy, her smile radiant. “But the system failed her too – why wasn’t her risk flagged earlier?” The UK’s maternity system, strained by a 15% midwife shortage (2,500 vacancies in 2023), struggles to support high-risk home births. NHS guidelines urge hospital delivery for women like Jen, but independent midwives, unregulated by the Care Quality Commission, operate in a gray area. Fielding, cleared of negligence, admitted she underestimated Jen’s rigidity. “Her plan was a masterpiece, but it didn’t account for chaos,” she said.
The tragedy has sparked fierce debate. On Mumsnet and X, posts under #HomeBirthTragedy oscillate between support for Jen’s autonomy and warnings about romanticizing natural birth. “She deserved better support, not judgment,” one user wrote, while another cautioned, “High-risk? Hospital is the only safe choice.” Experts like Dr. Hannah Patel, an obstetrician at King’s College Hospital, highlight the risks: “Home births can be safe for low-risk pregnancies with robust backup plans, but previous hemorrhages demand hospital-grade monitoring.” NHS data shows postpartum hemorrhage occurs in 6% of UK births, with 1 in 1,000 fatal without swift intervention.
Jen’s story resonates beyond Prestwich. In 2022, a similar case in Leeds saw a mother die after a home birth hemorrhage, prompting calls for tighter regulations. The Royal College of Midwives advocates for better risk assessments and mandatory hospital transfers for high-risk cases, but funding lags. Jen’s sister, Laura, 38, has launched a petition for “Jen’s Law,” demanding integrated care for home births: dedicated midwives, hospital backups within 15 minutes, and mandatory risk disclosures. It’s gained 20,000 signatures, fueled by a viral photo of Jen and Rudy finger-painting, Agnes’s ultrasound taped nearby.
The community’s grief is palpable. At a June 10 vigil in Heaton Park, 200 gathered, releasing white balloons for Jen and Agnes. Rudy, clutching Rob’s hand, placed a daisy on a makeshift shrine. Neighbors have rallied, delivering casseroles and funding Rudy’s therapy. “Jen was our sunshine,” said friend Emma Clarke, who runs a local mums’ group. “She planned everything, but no one plans for this.” Rob, sifting through Jen’s birth plan, found a note: “For Agnes, my wildflower, born free.” It’s now tattooed on his wrist, a vow to keep her memory alive.
The inquest, set to conclude in November 2025, probes systemic gaps: Why wasn’t Jen’s risk profile escalated? Could Fielding have pushed harder for transfer? Why do independent midwives lack oversight? Meanwhile, home birth advocates defend choice, citing studies showing 80% of planned home births in low-risk cases end safely. But Jen’s case wasn’t low-risk, a fact her plan couldn’t rewrite. Social media amplifies the divide: #JensLegacy trends with 50,000 posts, some praising her courage, others urging reform. A TikTok tribute, set to Enya’s “Only Time,” has 1.2 million views, showing Jen’s park photo dissolving into Agnes’s ultrasound.
For Rudy, the loss is a shadow he can’t name. “Mummy and Aggie are with the stars,” he told Rob, pointing skyward. Rob, navigating single parenthood, has quit his job to focus on Rudy, supported by a GoFundMe raising £75,000. He’s campaigning alongside Laura, speaking at maternity safety forums. “Jen wanted control, but the system should’ve caught her,” he said. The NHS has pledged £10 million for midwife training, but critics call it a drop in the bucket.
As Prestwich’s leaves turn golden, Jen and Agnes’s absence lingers – in the empty birthing pool, in Rudy’s unanswered questions, in Rob’s sleepless nights. Their story isn’t just a cautionary tale; it’s a mirror reflecting choice’s power and peril. Jen’s plan, a love letter to Agnes, now fuels a movement for safer births, ensuring no mother’s dream ends in darkness.
News
😭🎶 “I Couldn’t Breathe Anymore” — Neil Diamond, 84, Breaks Down in Tears as Hugh Jackman & Kate Hudson Sing the Song He Wrote in His Darkest Days
Neil Diamond remained perfectly still in the softly lit recording studio, his silver beard catching faint reflections from the monitor…
🚨💍💔 Married Just 7 Months… 😢💍🚨 They Survived When Four Others Died — But This Is the Cruel Price a Newlywed Couple Is Now Paying After Bolton’s Tragedy
Just seven months after exchanging vows in a dream wedding filled with laughter, promises, and endless hope, Georgina Daniels and…
🚨💔 “He Challenged Me” — The Terrifying Confession That Shattered the ‘Love Triangle’ Myth in the Anaseini Waqavuki Murder Case 😨
In the hushed corridors of a New South Wales courtroom, a single sentence uttered by the accused has sent chills…
📹💔 A Routine That Never Failed… Until It Did — Inside the Surveillance Video That Solved the Mystery of Chicago Teacher Linda Brown
In the tight-knit Bronzeville neighborhood of Chicago, where streetlights cast long shadows on quiet row houses and families know each…
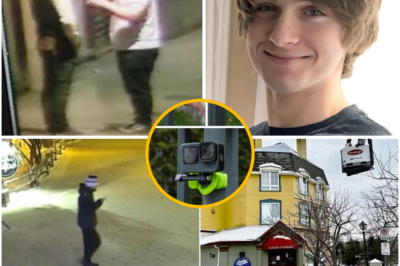
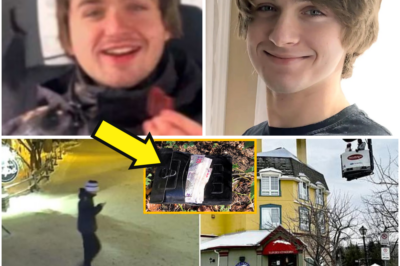
🍺🚓 Bar Staff Reveal Liam Toman Left the Venue Furious After a Physical Clash With a Man Described as a Regular, Then Was Never Seen Again
Nearly twelve months have passed since Liam Gabriel Toman, a bright and energetic 22-year-old from Ottawa, stepped out of Le…
🚨🏔️ A Dream Ski Trip Turns Into a Living Nightmare: Liam Toman Walked Alone From a Bar, Just Minutes From His Hotel Room, and Was Never Seen Again
A young man, full of life and promise, steps out from a bustling bar, his breath fogging in the cold…
End of content
No more pages to load